Exploring the empirical possibility that treatment delays and invasive ventilation contributed to US excess deaths in 2020
Evidence implicating unproven COVID-19 policies, propaganda, and panic as the real killers of 2020 continues to emerge, notably in the form of delayed treatment and improper mechanical ventilation
In 2020, the US recorded some 500,000 excess deaths, with significant excess deaths starting to accrue in the March/April period. Contrary to popular belief, SARS-CoV-2, the respiratory virus that causes the clinical cold/flu-like condition referred to as COVID-19, was not the primary driver of the excess deaths. Indeed, according to the latest genetic and antibody evidence, SARS-CoV-2 had been harmlessly circulating around the globe well before 2020. Moreover, WHO, CDC, and FDA definitions and data confirm that SARS-CoV-2 is a respiratory virus that lacks the inherent power to cause significant and sustained excess deaths in a country like the US. In fact, according to official data and definitions, SARS-CoV-2 may have caused or significantly contributed to around 50,000 deaths in the US in 2020, which may have been inflated by bad practices (see below). Instead, a confluence of unprecedented policies, propaganda and panic (PPP), initiated in the US in March 2020, served as the primary driver of excess deaths, including excess COVID-19 associated deaths. Much of this has been covered in my previous posts and by other authors, such as journalist Jordan Schachtel and medical expert Jonathan Engler.
While the aggregate number and general PPP cause(s) of the excess deaths recorded in 2020 are being made clear, specific casual pathways of excess deaths remain to be elucidated and quantified. In what follows, personal experience, expert testimony, and scientific research will be used to explore how PPP may have converged to drive excess COVID-19 suspected and associated deaths through a pathway of treatment delays and the misuse of intubation/ventilation.
My own personal experience during 2020/2021 suggests multiple causal pathways of excess death that involved treatment delays and/or medical mistreatment:
A woman in her late 70s with a neurodegenerative condition and who was living alone experienced pneumonia symptoms. Her doctor would only “see” her by phone and only reluctantly prescribed an empirical antibiotic at the urging of the woman’s son. No other instructions or care was provided. If not the for the commonsense care provided by her sons and aide, the woman would have died and become a statistic.
A woman in her 60s tested positive for SARS-CoV-2 and was symptomatic for COVID-19. A call to her doctor resulted in no care being provided. Her daughter, son, and son-in-law attempted to provide standard care that included such things as water, food, cold/flu medication, etc. Despite their best efforts, the woman needed to go to the ER to receive fluids. No other care was provided, and she was sent home.
A woman developed a gum infection. She was too scared by COVID-19 to see a doctor. She died from her gum infection.
A man of about 50 presented at the ER with a bought of diverticulitis. Due to COVID-19 protocols, his sibling was told that they could not accompany him into the ER. The nurse hooked him up to an IV of morphine and left the room. With no nurse present an no advocate by his side, he choked to death on his own vomit.
A man in his late 40s was battling cancer. He required properly dosed and delivered immunotherapy and the support of family and friends. Both needs were effectively denied to him due to COVID-19 protocols and panic. He died.
With the above in mind, in what follows an initial attempt is made to explore the roles that treatment delay and the misuse of invasive mechanical ventilation (IMV) may have contributed to excess deaths in 2020, as documented in peer reviewed scientific publications. Toward that end, we will start with some poignant comments delivered by Presidential candidate, attorney, and health freedom advocate Robert F. Kennedy Jr. in response to a question posed to him during a recent New Hampshire public forum,
“This is the first respiratory illness (COVID-19) in the history of medicine where you could go into the hospital with a positive PCR test and symptomatic, and the hospital will say there is nothing we’re going to do for you. You go home until your lips turn blue and until you can’t breathe and come back here, and we’re going to give you two things that will kill you, intubation and remdesivir.”
Our focus here will be on scientifically validating or invalidating Mr. Kennedy’s dual claim of treatment delay (“You go home until your lips turn blue and until you can’t breathe and come back here …”) and treatment harm through invasive mechanical ventilation (IMV) (“… and we’re going to give you two things that will kill you, intubation …”). Put simply, we will investigate what the relevant peer reviewed scientific literature has to say on both points.
With regard to the claim of treatment delay, Mr. Kennedy is essentially claiming that differential care of COVID-19 cases relative to historical respiratory virus cases resulted in significant treatment delays for COVID-19 cases, at least in the US. He seems to be claiming that COVID-19 cases presenting at health care facilities were told to go home, do nothing, and wait until they were hypoxic and needed emergency hospital care, while historically non-Covid patients were either admitted and received immediate hospital care, sent home with treatment instructions, or told to come to the hospital before their lips turned blue from hypoxia. Either way, the Covid-19 cases would receive delayed treatment (hospital or community based) compared to historical cases. Importantly, his claim can be empirically tested, at least in part, by comparing the time from symptom onset to hospital admission for historical non-COVID-19 respiratory cases and 2020 COVID-19 cases in the US.
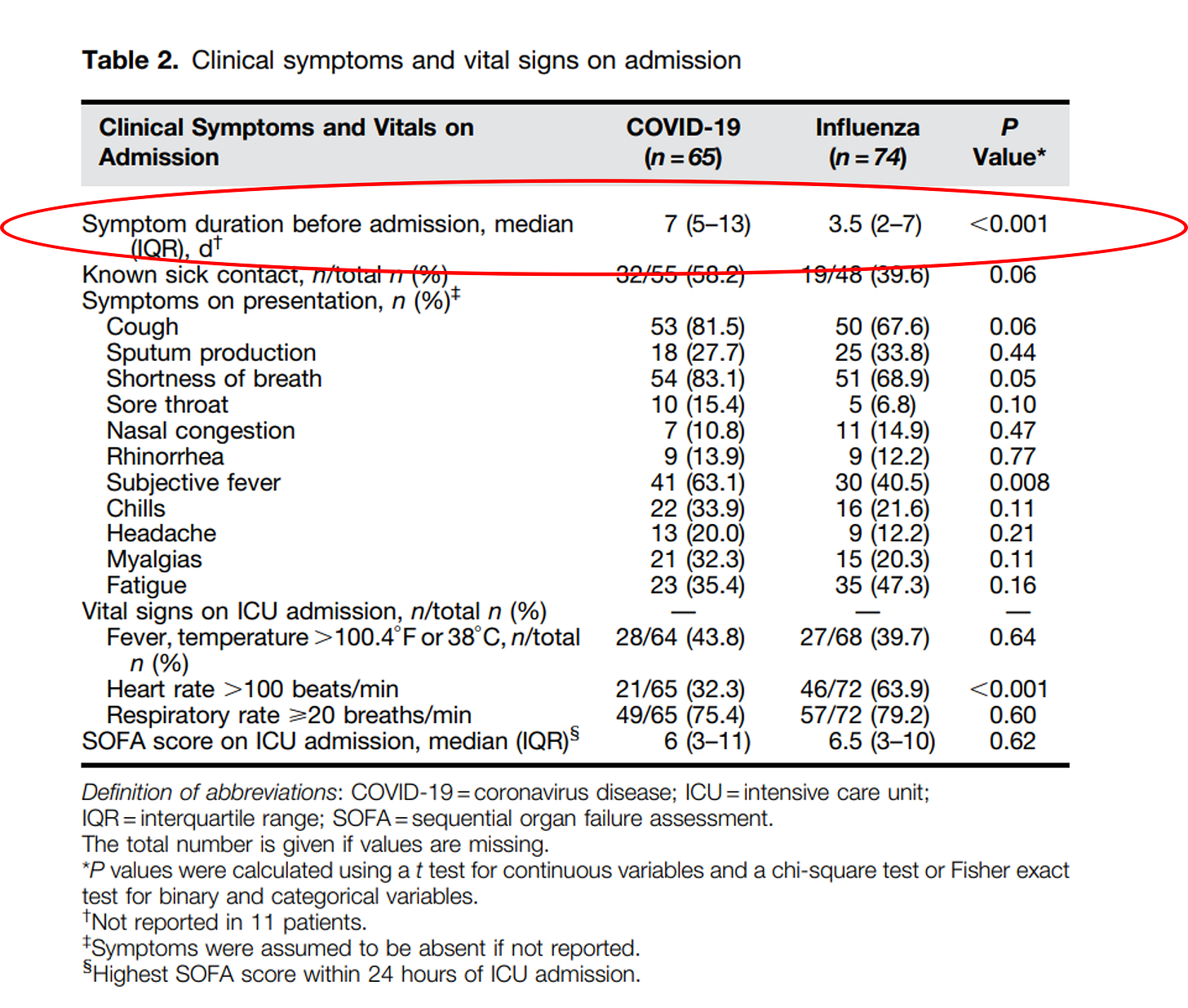
A search of PubMed turned up many broadly relevant and informative scientific articles, but only one article generated by the search was based on 2020 US data and also reported on symptom duration prior to health care facility presentation (hospital admission) for COVID-19 versus non-COVID-19 (influenza) respiratory cases. The article is entitled, “Comparison of Clinical Features and Outcomes in Critically Ill Patients Hospitalized with COVID-19 versus Influenza”. The following table (Table 2) is taken directly from the article,
The median time of symptom duration before hospital admission is 7 days for COVID-19 cases and 3.5 days for influenza cases. By one measure, the experienced treatment delay for COVID-19 cases relative to influenza cases is a highly significant 3.5 days. This confirms RFK Jr.’s claim of notable treatment delays for COVID-19 patients. What caused the treatment delay? Unfortunately, the study was not conducted to directly address that question. In the discussion section of the article, however, the authors mention and speculate about “several other factors” that “may have impacted outcomes in this study, including altered care processes and treatment protocols early during the pandemic.”
While not a US-based study, researchers from the UK also reported data on COVID-19 treatment delay in an article entitled, “Severe COVID-19 pneumonia in an intensive care setting and comparisons with historic severe viral pneumonia due to other viruses”. According to their data, COVID-19 patients experienced symptoms for 7 days prior to hospitalization while patients with non-COVID respiratory viral illness experienced only 4 days of symptoms prior to hospitalization, resulting in a highly significant 3-day treatment delay. The authors hypothesize that the treatment delay is because SARS-CoV-2 infection progresses more slowly than the other respiratory virus infections.
In an article entitled “Characteristics of patients with Coronavirus Disease 2019 (COVID-19) and seasonal influenza at time of hospital admission: a single center comparative study”, Swiss researchers reported that the time from symptom onset to hospital admissions was 7 days for COVID-19 patients and 3 days for influenza patients, which translates into a highly significant 4 day treatment delay. Importantly, the article’s authors discuss two hypotheses to account for the treatment delay, including the hypothesis that COVID-19 policies and procedures may have contributed,
“The variable that discriminated best between COVID-19 and influenza was the time between symptom onset until hospital admission. This finding probably reflects the fact that clinical deterioration commonly occurs on day 5 to 8 after symptom onset in COVID-19 patients, which then causes patients to seek medical care. This important difference between COVID-19 and influenza patients, which has previously been reported by another study [14], could be helpful in the early assessment of patients with ARI. We can however not exclude that public lockdown measures, which were in place during the time when most COVID-19 patients presented to our hospital, may have prolonged the time delay between symptom onset and hospital admission in some patients.”
In summary, a 2020 US study and two independent European studies provide confirmation of RFK Jr.’s claim of significant treatment delays for hospitalized COVID-19 patients relative to historical controls. All three studies point to a typical hospitalization treatment delay of about 3-4 days. The reasons for the observed delays remain to be fully elucidated. With that said, the authors of the Swiss study explicitly entertained the possibility that the treatment delay they observed, at least in part, may have been a consequence of policy decisions.
In light of the above, it should come as no surprise to learn that the first early and systematic treatment protocol for ambulatory COVID-19 patients (community cases prior to hospitalization) had to wait until January 2021 before being published in a peer reviewed journal. This implies that no formal COVID-19 outpatient treatment protocols existed during 2020 and that ambulatory COVID-19 patients had few medical options other than waiting to see if their lips turned blue followed by a hospital visit. In response to a critical comment that their proposed treatment protocol was dangerous, lead author Dr. Peter McCullough wrote,
“Empiric regimens [i.e., medical treatments based on small, potentially biased trials, weak observational studies, clinical experience, etc.] based on clinical judgment are not as “dangerous” as leaving patients untreated for many days only to succumb to calamitous hospitalization or death.”
Read that again: “leaving patients untreated for many days only to succumb to calamitous hospitalization or death.”
Dr. McCullough provided no citation or evidence in support of that bold assertion, treating it as common knowledge among medical experts. Apparently, in 2020 US medical doctors knew that COVID-19 treatment delay in the ambulatory setting was a real phenomenon, with potentially lethal consequences.
Now we will turn to the question of the role IMV may have played in causing excess US deaths in 2020, especially excess COVID-19 suspected or associated deaths. One study is particularly important in this regard. The study appears in the article “Non‑invasive ventilation versus mechanical ventilation in hypoxemic patients with COVID‑19” which was published in June 2021 and is based on March/April 2020 data from New York City (NYC).
The study compared mortality in hypoxemic (low oxygen) COVID-19 patients receiving IMV with those receiving non-invasive ventilation (NIV). The results are staggering. In unmatched and unadjusted analysis, IMV was associated with 10-fold increased odds of death (83% of patients died in the IMV group and 32% died in the NIV group). In matched and adjusted analysis, IMV was associated with an elevated odds of death of 8.0 compared to NIV. Patients with mild hypoxemia fared even worse on IMV relative to NIV. The authors of the study wrote,
“In this retrospective multi-center cohort study, we observed that MV (IMV) use in hypoxemic patients with SARS-CoV-2 infection was associated with a significantly higher odds of mortality over the course of respiratory intervention compared to NIV use. This outcome was consistent when accounting for differences in demographics, comorbidities, pharmacologic therapies, ICU status, and initial SpO2 level.”
It is sad to say, but the results of the NYC IMV/NIV study are consistent with RFK Jr.’s claim that intubation (IMV) of real or suspected COVID-19 patients practically amounted to hospitals “giving things that will kill you.”
Based on the claims made by RFK Jr., personal anecdotes, and the scientific data and expert commentary, it is not hard to imagine plausible scenarios involving unprecedented policy decisions, propaganda and panic – specifically in the form of treatment delays and the improper use of IMV - that contributed to excess COVID-19 suspected or associated deaths in 2020. In what follows, let us consider three such scenarios.
Scenario I: A person in a marginalized group starts to develop cold symptoms. The person contacts a community health care provider and is told to get tested for COVID-19. The person tests positive and reports back to the health care provider. The person is told to stay home until they have difficulty breathing. No other instructions or care is provided. The person does what they are told and finally presents to the ER with mild hypoxia. Due to fear and panic among hospital staff about SARS-CoV-2 transmission and poor information about treatment options, the hospital adopts a policy of never using non-invasive oxygen support and only using IMV, even on patients with only mild hypoxemia. The patient dies.
Scenario II: A person presents to the ER with mild hypoxemia and cold-like respiratory symptoms. Based on personal history the person is suspected of having but not PCR confirmed to have COVID-19. In keeping with CDC COVID-19 case definitions, financial compensation schedules for COVID-19 patients, and hospital policies, the person is placed on IMV. The patient dies.
Scenario III: An elderly person is living at home alone, with no means of transportation, and without the benefit of a health advocate. They develop cold symptoms. They manage to contact a community health care provider. The health care provider tells them to stay home. Because of media propaganda and personal fear, the health care provider assumes the person has COVID-19 and further assumes that no treatment options exist. Hence, the elderly person is told to stay home until they have difficulty breathing and to then call an ambulance. The person dies alone from dehydration.
Now repeat those and other scenarios across the entire country for 10 months in 2020. In a normal year, the health care system is estimated to cause approximately 200,000 deaths by medical errors. Is it really a stretch to think that from mid-March 2020 to the end of the year - a time of unprecedented panic, propaganda, and policy insanity – medical errors were significantly amplified, resulting in 2- or 3-fold as many iatrogenic deaths? On its face that seems to make more sense than blaming a cold virus with a 10% attack rate and 0.2% infection fatality rate that people had been living with uneventfully since well before March 2020 and right up to the edge when an emergency was declared, and insanity ensued.